Reference
Valle-Hita C, Salas-Huetos A, Fernández de la Puente M, et al. Ultra-processed food consumption and semen quality parameters in the Led-Fertyl study. Hum Reprod Open. 2024;2024(1):hoae001.
Study Objective
To determine if ultraprocessed food (UPF) consumption is associated with semen-quality parameters
Key Take-Away
Higher UPF consumption was inversely associated with total sperm count, sperm concentration, and total motility of sperm in Spanish men of reproductive age.
Design
Cross-sectional analysis
Participants
Investigators conducted this study using data from the first 200 healthy male participants (mean age 28 ± 5.5 years) enrolled in the Led-Fertyl Study (lifestyle and environmental determinants associated with the seminogram and other parameters related to male fertility). Prior studies have used this cohort to measure organic contaminants and industrial pollutants in semen.1
Study volunteers were excluded from participating for a variety of reasons including chronic disease, reproductive disorders or vasectomy, major organ transplantation, cardiovascular disease (CVD), human immunodeficiency virus (HIV) or hepatitis infection, acute infections or ongoing inflammation, active cancer or cancer history, psychiatric disorders, cirrhosis or liver failure, endocrine diseases, use of antidepressants, calcium channel blockers, alpha-adrenergic blockers, anti-epileptic drugs, antiretrovirals, immunosuppressive agents or cytotoxic agents, ongoing treatment with systemic corticosteroids, weight loss exceeding 5 kg within the past month, a history of alcohol or drug abuse, or any condition that could potentially impede adherence to the study protocols. The average age of these 200 participants was 28.4 years, and their average body mass index (BMI) was 24.4.
Study Parameters Assessed
Two parameters were compared: dietary intake of ultraprocessed foods and test results of sperm quality.
Participants completed a validated, 143-item food-frequency questionnaire via phone interviews. Investigators converted their responses for each food item into grams per day and used these data to compute total daily energy and nutrient intakes. They used the NOVA classification system to analyze this information for each study participant to determine consumption of UPF and the percentage of energy from UPF.
Investigators measured sperm quality from semen samples collected via masturbation from each participant. They evaluated macroscopic attributes, including semen volume and pH, and examined microscopic characteristics using a phase contrast microscope in conjunction with a computer-assisted sperm analysis (CASA) system. These assessments included sperm count, sperm concentration, sperm motility, sperm vitality, and sperm morphology.
Investigators also evaluated adherence to a Mediterranean diet using a 14-item Mediterranean diet questionnaire. They collected data on the frequency of consumption of extra virgin olive oil, butter, margarine, or cream, vegetables, fruits and juices, meat, fish, legumes, nuts, pastries, caloric and noncaloric artificially sweetened beverages, wine, etc. Overall score ranged from 0 to 14 points, meaning nonadherence or high adherence to the Mediterranean diet, respectively.
In-hospital medical assessments included anthropometric measurements, blood pressure, and biological samples (fasting blood and semen).
Primary Outcome
The study primarily assessed the association between UPF consumption and sperm quality.
Secondary outcomes were possible covariants that might also affect sperm quality. Investigators collected general lifestyle information (smoking habits and physical activity) and sociodemographic characteristics (age, education level, and income) through online questionnaires.
Key Findings
Sperm concentration (β: −1.42 x 106 spz/mL; 95% CI: −2.72 to −0.12) and motility (β: −7.83%; 95% CI: −15.16 to −0.51) were lower in participants in the highest tertile of UPF compared to the lowest.
Investigators observed similar associations for sperm count when they analyzed UPF per 10% increment of energy from UPF consumption (β: −1.50 x 106 spz; 95% CI: −2.83 to −0.17).
“Theoretically replacing 10% of energy from UPF consumption with 10% of energy from unprocessed or minimally processed food consumption was associated with a higher total sperm count, sperm concentration, total motility, progressive motility, and normal sperm forms,” the authors stated.
Transparency
The authors reported funding sources as from Spanish and European Union funding agencies, and no conflicts appear to exist.
Practice Implications and Limitations
Worldwide, about 10% of couples who desire to have children are afflicted with infertility. In about half of the cases (40%–50%), the semen is the issue, with either poor quality or low volume.2
There has been a striking decrease in semen quality reported in the last few decades. A 2023 systematic review and meta-regression analysis of semen samples collected worldwide described a decline that accelerates with each passing year. Between 1973 and 2018, sperm counts dropped by just under 52% globally. The data since 2000 reveals that the percent decline per year was even worse than prior decades, doubling from 1.16% post-1972 to 2.64% post-2000. Total sperm counts have dropped 62.3% since 2000.3
While no definitive explanation for this phenomenon has emerged, several likely explanations exist.
There is evidence that these trends are worse in developed and industrialized countries, suggesting that environmental and lifestyle factors probably play a role in the decline. There are further reasons to believe that these same factors play a role in semen quality because evidence suggests adhering to a healthy diet rich in unprocessed or minimally processed foods, such as fruits, vegetables, legumes, or nuts, while limiting the consumption of red and processed meat and sugar-sweetened beverages, is associated with improved semen quality.4
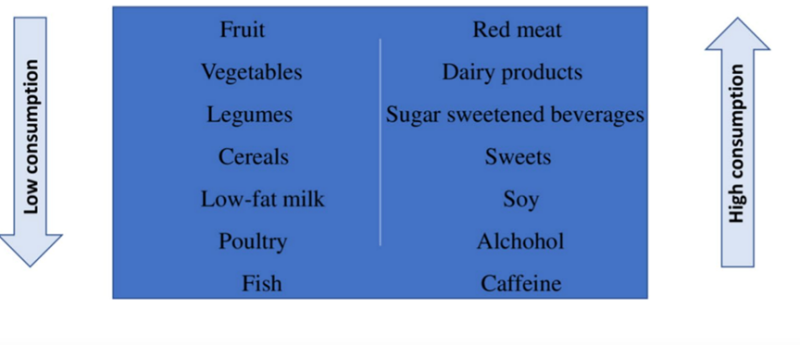
Figure: Eating habits associated with male infertility. Copyright Giulia Pecora, Francesca Sciarra, Elena Gangitano, and Mary Anna Venneri 2023.
A 2023 review by Pecora et al nicely sums up the data on how dietary habits and specific foods impact sperm quality. It reconfirmed that diets low in fruit, vegetables, legumes, low-fat milk, poultry, and fish are associated with poor semen quality and low counts. They report a similar impact for diets high in red meat, dairy products, sugar-sweetened beverages, sweets, soy, alcohol, and caffeine.5
Other evidence suggests that environmental pollution, illicit drug use, smoking, alcohol consumption, dietary exposure to potential endocrine-disrupting chemicals, psychological stress, and unhealthy diets are partly to blame for poor semen quality.6 It has been theorized that avoiding such exposures might benefit infertility.
Perhaps the largest factor and easiest-to-assess reason sperm counts are dropping is that body mass index is closely associated with semen quality. Increasing BMI is associated with increases in adipose tissue, which is predictive of aromatase activity that, in turn, leads to an increase in 17 beta-estradiol (E2). Increased E2 inhibits the hypothalamic-pituitary axis, consequently lowering gonadotropin-releasing hormone (GnRH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH).7 As a result, increasing BMI in males decreases testosterone and sex hormone binding globulin (SHBG) and increases free androgen and E2 levels. The reduced FSH stimulation affects Sertoli cell function and sperm production and lowers Leydig cell testosterone production. Bottom line is that as BMI increases, semen quality falls.8
As obesity rates are increasing globally,9 perhaps we need not dig deeper to explain this low-sperm phenomenon. It may be that any diet that lowers BMI will improve semen quality or, conversely, any diet associated with increasing BMI is bad news for semen production.
During the period in which sperm counts have dropped. the consumption of ultraprocessed foods has increased rapidly. Such foods are characterized by their poor nutritional quality and the inclusion of ingredients such as sugar, salt, fat, and food additives. Numerous papers have linked UPF consumption to various chronic diseases, including diabetes, hypertension, cardiovascular disease, and cancer. It is not clear whether this link is due to the presence of something in UPF or the absence in UPF of some valuable nutritional factor. It could simply be a combination of factors that leads to weight gain.
The general rule of thumb could be: ‘If you can’t make it in your own kitchen, don’t eat it.
This current study provides data to show that there is a significant association between consumption of UPF and worse sperm quality. What this study does not tell us is whether consuming UPF directly causes the drop in sperm counts or whether something else is going on.
To quote the study’s authors, “Cross-sectional studies do not permit the drawing of causal inferences.” In other words, just because the numbers yield statistically significant associations does not mean that they prove the relationship is causative. That is, we do not know that a diet high in UPF really causes the problem. The 2 events just seem to occur at about the same time, so we instinctively will jump to blame 1 for the other.
We can make a long list of changes that have occurred during the same period in which sperm counts and fertility have dropped, but this does not mean that these changes are responsible for the decline. While some people might believe that social media has caused these sperm-count drops and others might blame Velcro shoe closures, this doesn’t prove either phenomenon is responsible. The same can be said regarding UPF.
This isn’t the first, the only, or the last time we will face questions like this. Determining whether an association is causal is a recurrent challenge when reading epidemiological studies. Such studies are observational rather than experimental, and there are frequently multiple possible explanations for observed associations that look like cause-effect relationships. Causation needs to be distinguished from mere association. Observed associations might be due to 1 or more of the following factors:
- Chance (random error)
- Bias (systematic error)
- Confounding
- Reverse causality
- True causality
There is an epidemiological rule we should keep in mind as we read papers like this:
“An observed statistical association between a risk factor and a disease does not necessarily lead us to infer a causal relationship; conversely, the absence of an association does not necessarily imply the absence of a causal relationship.”
The bottom line when looking at epidemiological studies is that a “judgment about whether an observed statistical association represents a cause-effect relationship between exposure and disease requires inferences far beyond the data from a single study.”10
When we seek to judge causality, we often turn to a set of guidelines known as the Bradford-Hill Criteria, named for Sir Bradford Hill (1897–1991), an English epidemiologist famous for pioneering the use of randomized clinical trials in medicine. He is even more famous for demonstrating the causal connection between cigarette smoking and lung cancer.10,11
In the process of performing those smoking studies, Bradford Hill formulated a list of criteria that is still used to examine epidemiological associations. Although these criteria are not absolute but merely suggestions or hints, they help assess the information, even if they do not bring one to a clear yes-or-no answer. The “criteria” include the strength, consistency, specificity, temporal sequence, biological gradient, biological plausibility, coherence with current understanding, experimental evidence (if we remove the exposure, it alters the frequency of the outcome), and analogy (whether we know of something else with a similar effect so that we can say, “It works like…”) of the current knowledge about the association.
In this case, Bradford Hill won’t be that helpful for us because of the paucity of publications on this association. This study by Valle-Hita et al appears to be only the second to examine UPF and sperm quality.
An earlier study from 2022 compared the diets of 549 men diagnosed with asthenozoospermia (reduced sperm motility) against 581 normal controls. Men in the highest tertile of UPF intake were more likely to have asthenozoospermia (OR=1.53; 95% CI: 1.12, 2.10; P<0.05) than men in the lowest tertile.12 In the current study by Valle-Hita et al, it is suggested that a 10% shift in calorie intake away from UPF may make a significant difference in sperm quality.
With so little data, reaching conclusions about strength, consistency, specificity, or even temporal sequence of the association would be overreach; all we should currently say is the association has been reported and appears to be significant.
This UPF idea does seem biologically plausible as we know that diets “higher in UPF provide lower intakes of protein, total dietary fiber, monounsaturated and polyunsaturated fatty acids, and bring a higher intake of saturated fatty acids. Individuals consuming more UPF also showed a lower adherence to a Mediterranean diet, a lower consumption of vegetables, fruits, nuts, legumes, and whole cereals and a higher consumption of dairy products, pastry and bakery items, snacks, prepared food, and sauces and seasonings.” Basically, we might consider high intakes of UPF as a shorthand way to describe high adherence to a modern Western diet.13 The same health conditions associated with the Western diet can be directly ascribed to a high-UPF diet and rising rates of obesity.14
While there is scant evidence so far comparing UPF consumption to poor semen quality, there is ample evidence telling us that adherence to the Western diet is associated with poor sperm quality.15,16 Risk of asthenozoospermia increases with adherence to a Western diet.17 Specific food groups that we consider ultraprocessed and typical of the Western diet—for example, processed meats or sugar-sweetened beverages—are negatively associated with healthy sperm.18,19
It’s not totally clear what is going on or what the specific biological mechanisms are that link UPF and deteriorating semen quality. Clearly, UPF foods have a lot of negatives that we associate with poor health outcomes; they are high energy density, high in simple sugars, trans fatty acids, and sodium, and low in fiber and antioxidants compared to minimally processed foods, and these characteristics are already strongly suspected as having a negative influence on male fertility.20 High intake of trans fatty acids has been linked to poor semen quality in at least 3 papers.21,22,23
In the Valle-Hita study, the men with higher UPF intake had lower antioxidant intake, and it is well-proven that antioxidants are important for sperm health.24 Earlier studies have linked specific antioxidants, such as vitamins C and E, beta-carotene, and zinc, along with omega-3 fatty acids, to sperm quality.25,26,27
The new UPF study by Valle-Hita et al isn’t their first to suggest diet impacts semen quality. Nancy Babio, the principal investigator in the Valle-Hita study, was among the researchers who conducted a study published in 2019 comparing Mediterranean diet adherence and sperm-quality parameters in 106 men. Those in the upper tertile of diet adherence had better sperm than those in the lower tertile. Other researchers have reported similar findings.28
In the Valle-Hita study, investigators did not compare the data on Mediterranean diet adherence to sperm quality but rather employed it just as a means to assess the nutritional quality of a high-UPF diet. Unsurprisingly a high-UPF diet is low in nutritional quality. This is actually an important finding as some theories that explain the link between high UPF intake and health risks suggest that contaminants in ultraprocessed food (leftover from processing or leached from packaging) are responsible. The poor nutritional intake of a high-UPF diet is adequate to explain the resulting poor health and, in the case of the Valle-Hita study, the poor semen quality and by extension the infertility.
Studies like this one are not trying to tell us what the best diet is but rather what the best assessment tool will prove to be to determine if a person’s diet is affecting infertility.
How do we use all this information when working with an infertile couple, especially if we know that the blame rests on semen quantity or quality? A high BMI might be our first hint that altering the diet may help. The NOVA classification system of UPF might give us a quick measure of how much a modern Western diet is contributing to the high BMI vs lack of physical activity or other factors.
The concept of moving a patient away from habitual consumption of ultraprocessed foods may be a better starting point than the Mediterranean Diet, only because it is a simpler approach. Daily counts of UPFs in the diet, with the goal of eating fewer, may be an easy place to start. The general rule of thumb could be: “If you can’t make it in your own kitchen, don’t eat it.”
What we now call “real food” or once tried to call “natural food” is just a simple way to describe non-ultraprocessed foods. Compliance with the Mediterranean diet might lead to better health outcomes in the long term, but it might be easier to take small steps with some people and use the lowering of UPF consumption as their “gateway” to a healthier diet.
Currently using the NOVA classification system to score the amount of ultraprocessed foods consumed is 1 of the best predictors of how diet will impact health. Scoring adherence to a Mediterranean diet may be a more accurate predictor, but that’s not the point. Few members of the public pay this sort of close attention to the details of their diets. Most people who desire to eat a healthier diet typically opt for organic foods, avoiding genetically modified organisms (GMOs), gluten, animal products, and preservatives. The extent that their food choices have been ultraprocessed does not usually even make their list of concerns, and yet it may be a more accurate predictor of health outcomes than any of these other parameters people often use to guide their food choices.29
The idea that eating organic foods affects semen quality is considered a well-proven fact by many. This belief originated with a letter to the Lancet published in 1994 that described how the authors collected sperm samples from participants at a weekend seminar sponsored by the Danish Organic Farmers’ Association.30 These study participants appeared to have higher sperm concentrations than found in reference groups of blue-collar workers. A second, similar report by Tina Jensen followed in 1996 that also suggested that semen quality of men who were members of a Danish organic food association was superior to other men who weren’t members.31
However, in 1998 these findings were criticized by SB Larsen who pointed out a clear methodologic error. Men in the blue-collar “control group” were not overly eager to provide semen samples; only 25% to 50% did. A high percentage of those who did submit samples were concerned that they were not fertile based on their reported lengthy time periods in which their partners had not conceived. As a result, the sperm counts of the control groups may have been lower based on this unknown selection bias, which allowed infertile men to have been more likely to be included.32
While Jensen’s findings are frequently mentioned, a study that this same SB Larsen published in 1999 is mentioned less often. Larsen compared sperm characteristics between 87 organic farmers and 171 traditional farmers with this potential source of error accounted for, and “… no significant differences in conventional measures of semen quality were found between organic and traditional farmers.”33
Choosing to eat organic foods does not appear to make a noticeable difference in fertility and so, by extension, probably not on sperm quality either. Another Danish study, this one published in 2023, looked at consumption of organic food and fecundability (getting pregnant and having babies) among couples trying to conceive. Final analysis of data from 2,069 participants showed organic food consumption had no meaningful association with fecundability.34,35
However, pesticide residues do appear to lower semen counts. Rather than approaches that differentiate by organic vs nonorganic, simply modifying a nonorganic diet to avoid those fruits and vegetables that have been reported to have high pesticide residues is associated with better semen quality and higher sperm counts.36
Following various specific diets may also affect sperm counts. There is ample evidence in support of Mediterranean diets being beneficial to sperm counts.37 There is some evidence that a ketogenic diet might be helpful based on laboratory research with rats. A ketogenic diet can ameliorate some of the damage caused by a high-cholesterol, high-fat diet.38 Sperm use ketone bodies as an energy source, and a ketogenic diet seems to restore motility in semen damaged by toxic exposure to monosodium glutamate.39 Low-carbohydrate diets cause other problems in semen function, but at least in mice, these can be ameliorated with the co-administration of curcumin.40
Concerns have been raised that if vegetarians use soy as a protein source to replace meat, it may cause problems in sperm production due to the estrogenic effects from soy isoflavones. This worry is based on animal research.41 Yet a human trial suggests that above-average soy intake may be protective to sperm.42
Ultraprocessed food, even if labelled as organic, vegan, nonGMO, and all the other traits people now deem important, is still ultraprocessed food and likely equally detrimental to our health. Teaching patients to recognize and avoid ultraprocessed foods should be important for not just men hoping to sire children but for prevention of a wide range of other health conditions.






