Iodine is a dietary mineral required for the production of thyroid hormones, which are necessary for brain development in utero and during early childhood. Iodine deficiency is associated with thyroid dysfunction, and frank iodine deficiency during pregnancy can result in irreversible brain damage and other neurological abnormalities in infants. Scientific evidence pertaining to the consequences of mild-to-moderate iodine deficiency is less consistent, but emerging signals suggest that even moderate iodine deficiency during pregnancy and/or lactation is clinically meaningful. Clinicians who advise pregnant and lactating women play a key role in facilitating public health efforts to eliminate iodine deficiency in North America.
Abstract
Iodine is a dietary mineral required for the production of thyroid hormones, which are necessary for brain development in utero and during early childhood. Iodine deficiency is associated with thyroid dysfunction, and frank iodine deficiency during pregnancy can result in irreversible brain damage and other neurological abnormalities in infants. Scientific evidence pertaining to the consequences of mild-to-moderate iodine deficiency is less consistent, but emerging signals suggest that even moderate iodine deficiency during pregnancy and/or lactation is clinically meaningful. National Health and Nutrition Examination Survey intake data demonstrate that pregnant and lactating women in North America are at risk of insufficient iodine intake. For these reasons, the American Thyroid Association, Endocrine Society, and American Academy of Pediatrics recommend that all pregnant and lactating women supplement with a daily multivitamin that contains 150 µg iodine. This recommendation is supported by guidelines established by the dietary supplement industry to urge supplement manufacturers to include 150 µg iodine in multivitamins intended for pregnant and lactating women. Clinicians who advise pregnant and lactating women play a key role in facilitating public health efforts to eliminate iodine deficiency in North America by echoing the aforementioned recommendation and ensuring that products they recommend are compliant with industry guidelines.
Introduction
Iodine is a dietary trace mineral required by the thyroid gland for the production of the thyroid hormones triiodothyronine and thyroxine (T4). Thyroid hormones play a central role in regulating metabolic processes and as important determinants of health throughout life.1 Fetuses, newborns, and young children are particularly vulnerable to sequelae of low maternal thyroid hormone production because thyroid hormones are necessary for brain development in utero and during early childhood.
During pregnancy, normal maternal thyroid production will increase almost 50%.2 Sufficient iodine intake from diet and/or supplementation is necessary to support this increased demand.3 Several coinciding physiological changes increase iodine requirements during pregnancy.4 Increased thyroid hormone production is necessary to maintain maternal euthyroid state. The fetus is totally dependent on maternal transfer of T4 until about 20 weeks of gestation.5 Later in pregnancy, direct transfer of iodine to the fetus is required to support fetal thyroid hormone production and to meet nutritional requirements for growth and development. Concurrent with the increased physiological demand for iodine throughout pregnancy, there is also evidence of amplified maternal iodine excretion via increased renal clearance.6 Iodine requirements remain increased throughout lactation to support neurodevelopment in nursing infants. For these reasons recommended intake levels for iodine are higher for women who are pregnant and lactating. The Institute of Medicine recommends iodine intake at 150 µg per day for nonpregnant adults, 220 µg per day for pregnant women, and 290 µg per day for lactating women.7 The World Health Organization (WHO) similarly recommends 250 µg of iodine daily for pregnant and lactating women.8
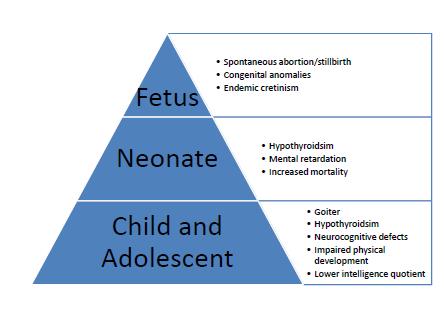
Healthy growth and development of fetuses and breastfed infants are dependent on sufficient maternal intake of iodine. When physiological requirements for iodine are not met during pregnancy and the first 2 to 3 years of life, a variety of functional and developmental abnormalities can occur. Conditions that result from inadequate iodine intake are grouped together as iodine deficiency disorders (IDD) and include hypothyroidism and goiter. IDDs that result from severe deficiency during pregnancy include cretinism and increased neonatal and infant mortality.9 Mild deficiency during pregnancy is associated with low thyroid function, learning impairment, and other minor neurocognitive defects that have been described in the literature (Figure 1).10,11
Figure 1. Iodine deficiency disorders.
Iodine Status
As recently as 2011, the International Council for the Control of Iodine Deficiency Disorders estimated that more than 2 billion people globally have insufficient iodine intake, including one-third of school-age children. Iodine deficiency remains the most prevalent, yet preventable, cause of irreversible cognitive impairment worldwide and is considered a public health problem in at least 32 countries.8 Iodine deficiency is more common in populations that live in isolated and mountainous regions of the world that are known to have low iodine levels in the food supply. North Americans are generally considered iodine sufficient; however, emerging evidence suggests that clinicians should be aware of the possibility of mild-to-moderate iodine deficiency in women capable of becoming pregnant.
Urinary iodine concentration (UIC) is a biochemical indicator of recent iodine intake, with median UIC used to assess the iodine status of a population. Threshold values for median iodine concentrations have been established to classify iodine status of populations and to identify populations at risk of deficiency. WHO defines adequate intake and adequate iodine nutrition as having a median UIC greater than 100 µg/L for nonpregnant women and greater than 150 µg/L for pregnant women. Mild-to-moderate deficiency during pregnancy is defined as having median UIC of 50 µg/L to 150 µg/L, and frank deficiency is defined as having median UIC below 50 µg/L.8
The recognition of trends toward reduced dietary iodine intake combined with increased physiological requirements during pregnancy and lactation have raised concerns about mild-to-moderate iodine deficiency impacting women of childbearing age in the United States.
Clinical use of UIC to evaluate individual iodine status in patients is not reliable due to diurnal variation in urinary iodine excretion. There is no clinical test that is considered a valid measure of individual iodine status. Some practitioners use other available tests, such as the 24-hour iodine/iodide challenge, the iodine skin test, or hair mineral analysis, but these tests have not been validated as reflecting iodine status of an individual and are based on several unproven assumptions.1,12
Overall data show that the US adult population is iodine sufficient; however, a subset of pregnant and lactating women may be at risk of deficiency. Intake data from the National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2008 suggest that iodine intake has decreased dramatically over the past several decades and by as much as 50% since the 1970s.13,14 During this period, the percentage of women of childbearing age with iodine deficiency rose from 4% to 15%. The NHANES data also indicate that over 35% of pregnant women have iodine levels considered to be moderately deficient,15 possibly placing their offspring at risk for IDD. Other studies of iodine status in pregnant US women have also reported marginal iodine deficiency during the first and second trimester (median UIC of less than 149 µg/L) and deficiency in 9% of pregnant women with UIC less than 50 µg/L.16 Apparently healthy pregnant women with UIC of 50 µg/L or less during the third trimester are significantly more likely to have infants who are small for gestational age than healthy women with UIC between 100 µg/L and 149 µg/L.16
The decline in iodine intake in the United States may have resulted from public health efforts control blood pressure by reducing sodium intake. Iodine has also been reduced as a dough conditioner and in dairy products, and the salt used in processed and convenience foods does not contain iodine. It is not uncommon for patients monitoring total salt intake to forgo using table salt—the most prevalent source of iodized salt—as a way to reduce overall sodium intake. Clinicians may consider other dietary variables that influence iodine intake. For example, a vegetarian or vegan diet can result in inadequate iodine intake unless adequate amounts of seaweed, a source of iodine, are consumed.17,18
Environmental chemicals also play a role in the decline of iodine intake. They interfere with iodine assimilation by competing for transport by the sodium iodide symporter (NIS) in the thyroid gland and lactating mammary gland. The NIS transports iodide into thyroid follicular cells for thyroid hormone synthesis, and in the lactating mammary gland it transports iodide into milk. Other strong anions found in the environment—such as thiocyanates, nitrates, and perchlorates—can compete with and replace iodine as a substrate for NIS transport across plasma membranes. Perchlorate’s affinity to NIS is 30 times greater than that of iodide, and perchlorate exposure raises concerns with regard to competitive inhibition of iodide uptake and decreased thyroid function.19 Ensuring adequate iodine intake in mother and child may reduce vulnerability to environmental agents that interfere with iodine uptake, which is in part why the American Academy of Pediatrics and Council of Environmental Health recommend a prenatal and lactation supplement with adequate iodide.20
Consequences of Iodine Deficiency
The consequences of severe iodine deficiency include adverse obstetric outcomes (ie, premature birth, spontaneous abortion, stillbirth), congenital anomalies, decreased intelligence, and neurological cretinism. Iodine supplementation during pregnancy in populations with prevalent severe iodine deficiency has been shown to improve outcomes, such as decreases in fetal mortality and endemic cretinism.21 Iodine deficiency has also been correlated with a general intellectual impairment across populations. An analysis of data from Chinese studies demonstrates that children with iodine deficiency have an average intelligence quotient (IQ) score 12.5 points lower than that of children with normal iodine levels.22 A separate combined analysis of several observational studies conducted in children indicates that chronic iodine deficiency is associated with impaired intellectual function, diminished fine motor skills, and reduced IQ scores.23 These data are observational and do not establish causality, but the totality of evidence and concerns about preventable causes of low intelligence have mobilized the scientific and public health communities to prioritize iodine deficiency as a health concern requiring attention.
The adverse effects of mild-to-moderate iodine deficiency during pregnancy and breastfeeding relating to cognitive outcomes in infants and children are not supported by rigorous randomized placebo-controlled clinical trials (RCTs). Experts have noted that conducting RCTs to establish a link between marginally inadequate iodine status in pregnant women and adverse cognitive outcomes in offspring would be unethical because RCTs, by design, would randomly assign some women at risk for mild-to-moderate iodine deficiency to the placebo group, which would not take iodine during the trial. In the absence of data from large scale RCTs, the totality of available evidence informs recommendations by medical organizations for iodine supplementation during pregnancy and lactation as a preventive public health measure to avoid consequences of mild-to-moderate deficiency.
Evidence to support iodine supplementation in pregnant and lactating women includes basic science and emerging clinical evidence. Clear evidence demonstrates that iodine, as a major structural component of thyroid hormones, plays a role in neuron and brain development during fetal and early postnatal life.7 Mechanistic data are further supported by evidence that mild hypothyroidism during pregnancy, characterized by low T4 and elevated thyroid stimulating hormone (TSH) levels, may result in delays in cognitive development in the offspring.24,25 Intervention studies have shown that iodine supplementation during pregnancy increases maternal iodine status, reduces maternal and neonatal thyroid volume, and reduces maternal TSH levels.26,27 It is noteworthy that not all trials have shown that perinatal iodine supplementation improves biomarkers of thyroid function,28 but evidence suggests improvement in measures of infant neurocognitive function when women living in geographic areas of mild iodine deficiency take an iodine supplement.29,30 Overall, the emerging evidence of benefit—considering the large margin of safety of the recommended iodine supplemental intake of 150 µg per day and in light of the median dietary iodine intake in women (190 µg-210 µg per day) and tolerable upper intake level for iodine (1,100 µg per day)—makes recommendations for perinatal iodine supplementation a prudent public health measure (Table).
IOM7 | Dietary iodine intake (median intake for women) | 190 µg/d- 210 µg/d |
IOM7 | RDA: nonpregnant females | 150 µg/d |
IOM7 | RDA: pregnant females | 220 µg/d |
IOM7 | RDA: lactating females | 290 µg/d |
WHO8 | Recommendation for pregnant and lactating females | 250 µg/d |
IOM7 | Tolerable upper level: (includes adult pregnant and lactating women) | 1,100 µg/d |
Table. Considerations for Iodine Supplementation in Women
Abbreviations: IOM, Institute of Medicine; RDA, recommended dietary allowance; WHO, World Health Organization.
Iodine Supplementation for Pregnancy and Lactation
The impact of iodine deficiency on intelligence has been recognized for more than 150 years. Publications dating as far back as the 1830s suggested that salt fortified with iodine was necessary for good health in people living in mountainous regions of Europe.21 Pioneering work of Swiss doctors established that iodine deficiency was the cause of endemic goiter and its clinical manifestations.31 The effect of iodine deficiency on children’s intelligence and subsequent effects on the workforce and economy in various regions of the world have led to international public health efforts to eliminate iodine deficiency worldwide.
Over the past 75 years, the international public health community has reduced the global burden of IDD through coordinated programs aimed to control and prevent iodine deficiency. As early as the 1960s, WHO developed programs to characterize the extent of the problem and engage governments of impacted regions, but these efforts were not well coordinated, so the problem of iodine deficiency was not addressed in a consistent way. In the late 1980s, as policymakers became better informed about the significance of iodine deficiency and its preventable nature, support for global initiatives increased. A turning point in the global efforts to eliminate IDD was the 1990 United Nations (UN) World Summit for Children, which resulted in strategies and goals to eliminate iodine deficiency. These strategies were approved by 159 countries at the joint Food and Agriculture Organization of the UN/WHO International Conference on Nutrition in 1992. In 2002, the prevention of iodine deficiency was still a public health priority as the UN General Assembly’s special session on children endorsed the goal of IDD eradication by the year 2005. Despite the success of these coordinated efforts, iodine deficiency and its complications still affect about 30% of the population globally, and iodine deficiency remains the leading preventable cause of mental retardation worldwide.32
The US population is generally sufficient in iodine15; however, the recognition of trends toward reduced dietary iodine intake combined with increased physiological requirements during pregnancy and lactation have raised concerns about mild-to-moderate iodine deficiency affecting women of childbearing age in the United States. The prevalence of marginal iodine deficiency in United States and the potential for avoidable adverse health and socioeconomic consequences have resulted in public health efforts by several US medical organizations to recommend that pregnant and lactating women supplement with a daily multivitamin with enough iodine. The American Thyroid Association,33 Endocrine Society,34 and American Academy of Pediatrics,20 have engaged in public health efforts to eliminate iodine deficiency during pregnancy. These groups have established policies and practice guidelines recommending that women in North America receive a dietary supplement containing 150 µg iodine daily during pregnancy and lactation. They also called on the dietary supplement industry to join their efforts by formulating multivitamins intended for use during pregnancy and lactation to contain daily doses of 150 µg iodine.
Survey data demonstrate that currently few US women adhere to iodine intake guidelines, with only 20% of pregnant and 15% of lactating women taking a dietary supplement with the recommended level of iodine.14 The high number of women not supplementing with enough iodine is due, in part, to lack of iodine in multivitamins. It is estimated that approximately 50% of prescription and nonprescription prenatal multivitamins do not contain iodine as an ingredient.14 Furthermore, a published analysis of the iodine content of prenatal products that included iodine as an ingredient shows that some products did not contain the amount listed on the label, with most variability found in products that used kelp, as opposed to potassium iodide, as the source of iodine.14 These data not be valid, however, because the application of analytical methods validated for testing iodine levels in urine to the testing of iodine levels in finished dietary supplements may not be appropriate.35 The author’s personal communications with experts in dietary supplement manufacturing and quality control confirm that the iodine content of kelp can fluctuate depending on growing conditions but also affirm that the iodine content of kelp can be standardized. This means that kelp can be used as a reliable source of iodine if proper quality controls are applied during manufacturing.
The American Thyroid Association’s advocacy efforts include outreach to the dietary supplement industry to explore ways to ensure that multivitamins intended to meet the nutritional needs for pregnant and lactating women contain 150 µg of supplemental iodine. The Council for Responsible Nutrition (CRN), the leading trade association for the dietary supplement industry, recognizes the importance of supporting efforts to improve iodine intake in populations at risk for deficiency. CRN supports the science-based recommendations of the American Thyroid Association, Endocrine Society, and American Academy of Pediatrics and also recognizes that the federal Women, Infants, and Children Nutrition Program recommends that all prenatal multivitamins provided by its program contain 150 µg of iodine per daily serving. In alignment with these organizations, CRN developed guidelines recommending that all manufacturers and marketers of multivitamin/mineral supplements for pregnant and lactating women in the United States include enough iodine to achieve supplemental iodine intake of 150 µg per day to support normal cognitive development in children (Figure 2).36
Dietary supplement manufacturers and marketers should include a daily serving of at least 150 µg iodine in all multivitamin/mineral supplements intended for pregnant and lactating women in the United States. |
Any safe and suitable iodine-containing dietary ingredient may be used as the source of iodine in such products when used in accordance with current Good Manufacturing Practice regulations for dietary supplements that ensure that the product consistently meets label claim. |
Figure 2. Council on Responsible Nutrition recommended guidelines for iodine quantity in multivitamin/mineral supplements for pregnancy and lactation.
Conclusion
Ensuring sufficient iodine intake in pregnant and lactating women is an important public health goal in the United States. To accomplish this goal in the absence of valid clinical tests for individual iodine status, all clinicians should adhere to current clinical guidelines and recommendations from authoritative medical organizations. Clinicians should advise pregnant and lactating women to take a dietary supplement containing a daily dose of 150 µg iodine. These efforts are supported by dietary supplement industry guidelines aimed at ensuring that dietary supplements intended for pregnancy and lactation contain sufficient iodine. Healthcare providers can further support public health efforts to ensure adequate iodine intake in pregnancy and lactation by insisting that any dietary supplement or prescription prenatal product they recommend contains a daily serving of 150 µg iodine.
Acknowledgements
The authors thank Alex Stagnaro-Green, MD, MHPE, and the American Thyroid Association for their iodine advocacy. Stagnaro-Green encouraged the Council for Responsible Nutrition to develop iodine guidelines as part of a collaborative public health effort to ensure that pregnant and lactating women supplement with iodine.
Editor's note: This article was updated 8/11/15.