The Prevención con Dieta Mediterránea (PREDIMED) study was the largest prospective randomized controlled experiment examining the effects of a Mediterranean style diet ever conducted. It may be the most valuable clinical trial on diet ever performed. It is important for us to understand the knowledge gained from both the original report and the subsequent publications derived from study cohorts.
Abstract
The Prevención con Dieta Mediterránea (PREDIMED) study was the largest prospective randomized controlled experiment examining the effects of a Mediterranean style diet ever conducted. It may be the most valuable clinical trial on diet ever performed. It is important for us to understand the knowledge gained from both the original report and the subsequent publications derived from study cohorts.
Introduction
The primary goal of the PREDIMED trial was to examine the effect of the Mediterranean diet on cardiovascular disease (CVD); these main findings were published in February 2013.1 This was the study that the media summarized as “eating a Mediterranean diet cuts risk of heart attacks and stroke by a third.” Since then, the data from the PREDIMED study have been used to power a number of other studies that have both confirmed the initial findings and provided additional information of value. The purpose of this article is to review the knowledge gained since PREDIMED was first published in February 2013.
The Original Study
PREDIMED was a large multicenter trial conducted in Spain in which participants who were at high cardiovascular risk (but with no CVD at enrollment), were randomly assigned to 1 of 3 arms: a Mediterranean diet supplemented with extra-virgin olive oil (EVOO), a Mediterranean diet supplemented with a mixture of nuts, or a low-fat control diet.
A total of 7,447 participants were enrolled in the study; 57% were women, and the mean age of participants was approximately 67 years at the start. As mentioned, all study participants were at high risk for CVD: about one-half were taking angiotensin-converting-enzyme inhibitors; one-fifth were taking diuretics; slightly more than one-fourth were taking other antihypertensive agents; two-fifths were taking a statin lipid-lowering drug; and over one-third were taking an oral hypoglycemic agent or insulin. The EVOO group started with 2,543 participants, the nut group 2,454, and the control group 2,450.
While the initial findings were of great interest and valuable for our patients, I was among those critical of the interpretations made when making comparisons among the 3 dietary groups. In the 2 years since the initial findings were published, new studies have appeared using more specific analyses that put these concerns to rest.
Participants in both of the 2 Mediterranean diet groups received dietary counseling individually and via group sessions at their first visit and then every 3 months for the duration of the study. They were given, without charge, 1 L of EVOO each week (approximately 2 oz per day) or 30 g of mixed nuts per day (15 g walnuts and 7.5 g each almonds and hazelnuts). The control group received small nonfood gifts. The Mediterranean diet groups were encouraged using dietary screening to adhere to their prescribed diet. The control group was encouraged to follow a low-fat diet. This control group initially did not have regular counseling with dieticians, though they did receive regular mailings encouraging compliance. After 3 years, this omission was seen as a methodological weakness and moving forward, the control group was also counseled by a dietician.
In the primary study, the endpoint was the rate of major cardiovascular events (myocardial infarction [MI], stroke, or death from cardiovascular causes).
On the basis of the results of an interim analysis, the trial was stopped earlier than planned, after a median follow-up of only 4.8 years. A primary endpoint had already occurred in 288 participants that varied significantly between groups. The relative risk (RR) for CVD was reduced by approximately 30% among the 2 groups who followed the Mediterranean diet. More specifically, those supplementing with EVOO had a 30% lower risk of having a cardiovascular event and those supplementing with nuts had a 28% lower risk than the low-fat control group.1 The data appeared to strongly suggest there was benefit in the Mediterranean diet: the multivariable-adjusted hazard ratios (HRs) for cardiovascular diseases/events were 0.70 (95% confidence interval [CI]:0.54-0.92) and 0.72 (95% CI:0.54-0.96) for the group assigned to a Mediterranean diet with EVOO (96 events) and the group assigned to a Mediterranean diet with nuts (83 events), respectively, vs the control group (109 events).
This study was the first major prospective trial designed to investigate the effects of the Mediterranean diet. Earlier evidence had been garnered from epidemiological studies and not randomized controlled trials. The Lyon Heart Study published in 1999 is the exception; it reported that following a Mediterranean diet reduced rate of a recurrence in individuals who had suffered a first MI.2
The Initial Data
It appeared that the Mediterranean diet worked—until the study details are carefully examined. In reality, the study was more about the impact EVOO and nuts had on the study population than what effect dietary changes had.
One important message hidden in the data was just how difficult it is to change a person’s diet. Recall that the study participants were at high risk for disease, most were already on medications to lower cholesterol, blood pressure, and/or blood sugar. They should have been “motivated.” Estruch and colleagues employed all the tools they could to encourage dietary changes. Yet just because study participants were encouraged to follow particular diets doesn’t mean they did. The study participants changed their diets only slightly, even with quarterly counseling sessions and encouragement from dieticians. Over the nearly 5 years of the trial, the only significant changes made by the 2 Mediterranean diet groups were in fish and legume consumption; fish consumption increased by 0.3 servings per week and legumes by 0.4 servings per week in comparison to the control group. No other changes reached statistical significance, except for EVOO or nut consumption.
Few of us would believe that eating one-third of a serving of fish and less than one-half a serving of beans per week more would be enough to have an impact on CVD. Belin reported in 2011 that 5 servings of fish per week would be required to see a similar 30% decrease in CVD risk.3 The decrease in CVD was likely related to the increase in nut or EVOO consumption rather than greater adherence to the prescribed diet than in the control group.
Although the control group was counseled to follow a low-fat diet, they were hardly compliant. The percentage of total energy from fat in the diet dropped from 39% to 37%, a nonsignificant decrease of 1.96% over the course of the trial.1 No conclusions can be drawn about the impact of switching to a low-fat diet from the initial study’s data analysis. One year into the study, nearly 92% of the low-fat diet control group reported that olive oil was the primary culinary fat in their diets. After 5 years, this consumption level had increased to more than 96%. More than 58% of the control group on the low-fat diet reported consuming more than 4 T (approximately 2 oz) of olive oil per day. This implies that any difference in CVD risk between groups was probably from the type of olive oil, “regular” vs EVOO.
There were significant differences in nut consumption between the experimental and control groups. At the end of the trial, nearly 91% of the nut group reported eating 3 or more servings of nuts a week while less than 17% of the control group ate that many. Again, what the data from the initial evaluation of this cohort tells us is the benefits of switching from regular olive oil to EVOO or eating a lot more nuts; this was not a comparison of a Mediterranean diet vs a low-fat diet.1
While these initial findings were of great interest and valuable for our patients, I was among those critical of the interpretations made when making comparisons among the 3 dietary groups. In the 2 years since the initial findings were published, new studies have appeared using more specific analyses that put these concerns to rest. At the same time, they refine other important findings from the PREDIMED data and have generated valuable knowledge. A current PubMed search yields more than 70 citations that have utilized PREDIMED data that have been published since this initial study in February 2013.
Slicing Through the Data
The PREDIMED trial was conducted in Spain, where the prevalence of a Mediterranean diet is higher than in other geographical regions. While the original design found little difference in dietary patterns of the 3 arms, there were measurable differences at baseline. Given that the groups changed their diets very little, the baseline diets at time of enrollment could be used to make assumptions about each participant’s dietary habits. A secondary analysis of the data in September 2014 divided the participants in the original study into 2 major groups based on the individuals’ dietary patterns at baseline, before they started the study. One group had a diet full of “red and processed meats, alcohol, refined grains and whole dairy products”4 labeled a Western dietary pattern (WDP), and the other had a diet that aligned with a Mediterranean-type dietary pattern (MDP).
This secondary analysis calculated HRs based on actual adherence to a MDP rather than to which study arm the people had been initially assigned. Using these more accurate dietary pattern groups, the PREDIMED data were then mined to give HRs using the various objective parameters measured in the study participants. This secondary analysis confirms the initial hypothesis about the impact of a Mediterranean style diet on CVD. It also brings to light the benefit of a MDP on metabolic syndrome (MetS) and diabetes. Lastly, it allows more focus on specific nutrients or foods found in a MDP and their effect on disease.
Comparing upper vs lowest quartiles of adherence, those who followed a Mediterranean style diet were 48% less likely to have a CVD event and 47% less likely to die during the course of the study than those who didn’t (adjusted HR:0.52; 95% CI:0.36-0.74; P-trend <.001) and all-cause mortality (adjusted HR:0.53; 95% CI:0.38-0.75; P-trend <.001). Again this new analysis ignored which original arm of the PREDIMED participants had been assigned to—low-fat, nuts, or EVOO—but just looked at how they actually ate.
These findings are stronger than the initial findings based on group comparisons. To say it simply, risks were cut in half. The closer a person’s diet matched what was defined as a WDP, the greater the risk of dying.4 Dietary adherence was assessed using a 14-point questionnaire.5
A clearer understanding of mechanisms that underlie the benefits of a Mediterranean diet has increased our confidence in these findings. A September 2013 paper reported that, “One of the mechanisms by which [Mediterranean style diet], particularly if supplemented with EVOO, can exert health benefits is through changes in the transcriptomic response of genes related to cardiovascular risk.”6 This was followed in September 2014 by a paper that explained these benefits are due to the impact of “dietary polyphenols on plasma nitric oxide and blood pressure.”7 Comparing blood pressure, plasma nitric oxide (NO) and urinary polyphenol excretion, both systolic and diastolic blood pressure decreased in proportion to the increased total polyphenol excretion and NO produced by either nuts or EVOO consumed. The researchers concluded, “The statistically significant increases in plasma NO were associated with a reduction in systolic and diastolic BP levels, adding to the growing evidence that polyphenols might protect the cardiovascular system by improving the endothelial function and enhancing endothelial synthesis of NO.”7
The initial PREDIMED report was a bit muddied because participants in all 3 original arms of the study consumed large amounts of olive oil. A May 2014 publication helped clear this up. It found study participants who were in the upper tertile of olive oil consumption at study baseline, regardless of which arm they were randomized into,
had 35% (HR:0.65; 95% CI:0.47 to 0.89) and 39% (HR:0.61; 95% CI:0.44 to 0.85) cardiovascular disease risk reduction, respectively, compared to the reference. The higher baseline total olive oil consumption was associated with 48% (HR:0.52; 95% CI: 0.29 to 0.93) reduced risk of cardiovascular mortality. For each 10 g/d increase in extra-virgin olive oil consumption, cardiovascular disease and mortality risk decreased by 10% and 7%, respectively.8 [Note: 10 g of oil is about 10 mL or about 2 t.]
Another May 2014 paper also individualized the data analysis and reported that greater adherence to a MDP was associated with positive changes in biomarkers of heart failure. The more an individual moved his or her diet toward a MDP and away from a WDP, the lower “their N-terminal pro-brain natriuretic peptide compared with those assigned to a low-fat diet. The same was found for in vivo oxidized low-density lipoprotein and lipoprotein(a) plasma concentrations.”9 The authors state that a Mediterranean style diet may “mitigate against risk factors for heart failure.”9
Another paper published the same month provides more detail on the underlying mechanics of this benefit. Greater adherence to a MDP produced desirable effects on “cyclooxygenase-2 (COX-2), interleukin-6 (IL-6), apolipoprotein A2 (APOA2), cholesteryl ester transfer protein plasma (CETP), and transcription factor 7-like 2 (TCF7L2) gene polymorphisms.”10
I will comment at length in a forthcoming issue of this journal on the July 2014 report that consumption of EVOO among PREDIMED participants was associated with a reduced incidence of atrial fibrillation (AF).11 EVOO appeared to confer reduced risk of AF in the original study groups of the PREDIMED study. Compared to the control group, the Mediterranean diet with EVOO group had a significant 38% reduction in AF risk (HR:0.62; 95% CI:0.45-0.85). The decrease in AF in the group following the Mediterranean diet with nuts did not reach statistical significance (HR:0.89; 95% CI:0.65-1.20). Given that 1 in 4 people will suffer from AF at some point in their lives,12 any intervention that reduces this occurrence will be of significant benefit to a large number of patients. Making sure that patients buy EVOO in lieu or “regular” olive oil seems a simple substitution.
Several papers have used the PREDIMED data to look at specific genetic polymorphisms that impact CVD risk and how they interact with diet. Ultimately, the individuality of CVD risk profiles lies in such minutiae. While there is limited clinical utility at this time, it is interesting to see that dietary choices can have synergy or detriment based on existing gene expression patterns.
A July 2014 publication looked at the effect diet has on the MicroRNA-410 regulated lipoprotein lipase variant rs13702. The rs13702T>C gene polymorphism impacts triglyceride levels and interacts with dietary fats in a beneficial manner to lower stroke incidence. Although this gene polymorphism may have benefited everyone in the study who had it, the impact only reached statistical significance in those following a MDP, as the diet and the gene appear to have a synergistic benefit. Having the C allele was associated 42% decrease in stroke risk in those assigned to the MDP (HR:0.58; 95% CI:0.37-0.91; P=.019 in C compared with TT carriers), while it was associated with a nonsignificant 6% reduction in the control group (HR:0.94; 95% CI:0.55-1.59; P=.805).13
Adherence to the MDP affects another gene involved in CVD, the XIPL-rs3812316 variant. This gene variant is protective against CVD, in general by lowering triglycerides. A February 2014 publication reported that adherence to the MDP was associated with significant increases in this protective effect: “the protection [from lower triglycerides] was stronger (odds ratio, 0.63; 95% CI, 0.51-0.77; P=8.6×10(‒6)) than when adherence to MedDiet was low (odds ratio, 0.88; 95% CI, 0.70-1.09; P=0.219).”14 In those with the protective allele following a MDP, risk for MI was 66% lower than those not (HR:0.34; 95% CI:0.12-0.93; P=.036 and HR:0.90; 95% CI:0.35-2.33; P=.830, respectively).14
A Meta-analysis
A meta-analysis published in July 2014 that examined olive oil consumption and risk of heart disease and stroke and combined data from case-control, cohort, and intervention studies is of interest as the results are in close approximation with these PREDIMED studies. Data from a total of 101,460 individuals and 38,673 people who had suffered strokes were combined. Analysis found a RR for stroke of 0.73 (95% CI:0.44-1.21) in case-control studies for a 25 g (approximately 1.6 T) increase in olive oil consumption. Cohort studies showed a RR of 0.74 (95% CI:0.60-0.92). The random-effects model combining all cardiovascular events—coronary heart disease (CHD) and stroke— showed a RR of 0.82 (95% CI:0.70-0.96). These findings suggested “an inverse association of olive oil consumption with stroke (and with stroke and CHD combined), but no significant association with CHD. This finding is in agreement with the recent successful results of the PREDIMED randomized controlled trial.”15
Less esoteric and perhaps more comprehensible to the public are the changes seen on ultrasound examination of carotid arteries. A February 2014 paper reported the results of measuring the intima-media thickness and plaque (ICA-IMT) in PREDIMED study participants. Halfway through the study period—that is after only 2.4 years—significant differences were seen in the arm supplementing their diet with nuts. The “ICA-IMT progressed in the control diet group” while it regressed in the nut group. No changes were seen in the EVOO arm: that is, no worse and no better.16 These new studies all confirm and lend growing weight to the idea that “[t]he results of the PREDIMED trial demonstrate that a high unsaturated fat, antioxidant and anti-inflammatory diet plan such as the Mediterranean diet is a useful tool in reducing overall mortality and in preventing cardiovascular disease.”17
Nuts and Mortality
Adding nuts to the diet clearly makes a big difference. Adding nuts is associated with a reduction in waist circumference and shifts in lipoproteins that are associated with a lower risk of heart disease, according to an October 2013 PREDIMED-based paper. PREDIMED participants in the nut group had a 2-in mean decrease in waist size. In addition, significant increases in the size of low-density lipoprotein particles and increases in high-density lipoprotein (HDL) concentrations were also reported.18
A July 2013 PREDIMED publication reported that nut consumption was associated with a significantly reduced risk of all-cause mortality (P-trend<.05, all). Compared to nonconsumers, participants consuming more than 3 servings of nuts per week had a 39% lower mortality risk (HR:0.61; 95% CI:0.45-0.83). A similar protective effect against cardiovascular and cancer mortality was observed. Participants allocated to the “Mediterranean diet with nuts” arm of the study who had already consumed more servings of nuts per week at baseline had the lowest total mortality risk, a 63% reduction (HR:0.37; 95% CI:0.22-0.66).19
Metabolic Syndrome and Diabetes
It isn’t only CVD that MDP benefits. One of the most interesting findings to come out in the last 2 years is that MDP diet has a beneficial impact on MeS and diabetes.
The first of these papers was published in March 2013 and reported that a high white blood cell count (WBC) serves as an early risk marker for developing MetS. Of the 4,377 participants in the PREDIMED study, 62.6% were already diagnosed with MetS at baseline and excluded from the WBC/MetS association. During a median follow-up of 3.9 years, anthropometric measurements, blood pressure, fasting glucose, lipid profile, and WBC counts were assessed yearly. Participants in the upper quartile compared to the lower quartile of WBC counts had an increased risk of developing MetS (odds ratio [OR]:2.47; 95% CI:2.03-2.99; P-trend<.001). This association was observed for all WBC subtypes except basophils. Compared to participants in the lowest quartile, those in the top quartile of leukocyte, neutrophil, and lymphocyte count had an increased risk of MetS diagnosis. Leukocyte and neutrophil count were found to be strongly associated with the MetS components hypertriglyceridemia and low HDL-cholesterol.20
An April 2013 paper reported that the MDP reduces oxidative damage to lipids and DNA in MetS and recommended this diet as a useful tool in MetS management.21
EVOO and nuts along with a MDP may lead to MetS reversion, suggesting that an energy-unrestricted Mediterranean diet may be useful in reducing the risks of central obesity and hyperglycemia in people at high risk of CVD. A secondary analysis of the PREDIMED data published in November 2014 looked at the effect of diet on incidence and reversion of MetS. According to this report, 960 participants—that is 50% of the 1,919 participants who did not have MetS at baseline—developed MetS during the course of the PREDIMED study. The risk of developing MetS did not differ between participants assigned to the various original arms, the low-fat control diet or those following either of the Mediterranean diets (control vs EVOO: HR:1.10; 95% CI: 0.94-1.30, P=.231; control vs nuts: HR:1.08; 95% CI:0.92-1.27, P=.3).
Interestingly, reversion or normalization occurred in 958 (28.2%) of the 3,392 participants who had MetS at baseline. Looking at this subset, compared with the control group, participants on either the EVOO-supplemented or the nut-supplemented arm were more likely to undergo reversion (control vs olive oil: HR:1.35; 95% CI:1.15-1.58, P<.001; control vs nuts: HR:1.28; 95% CI:1.08-1.51, P<.001). Participants in the group receiving EVOO supplementation showed significant decreases in both central obesity and high fasting glucose (P=.02); participants in the group supplemented with nuts showed a significant decrease in central obesity.
Just 1 year into the PREDIMED trial, differences in the blood plasma of participants was evident. The EVOO group “had significantly increased plasma concentrations of palmitic and oleic acids, but reduced proportions of margaric, stearic, and linoleic acids. Subjects in the nut group showed significantly increased levels of palmitic, linoleic, and ?-linolenic acids, but reduced proportions of myristic, margaric, palmitoleic, and dihommo-α-linoleic acids.”22 Increases in biomarkers from foods supplied to the Mediterranean diet arms—oleic and α-linolenic acids—were beneficially associated with the incidence, reversion, and prevalence of MetS.
The nut-supplemented and EVOO-supplemented arms had changes in plasma fatty acid composition that appear beneficial in the MetS.22 Thus, for patients with MetS, it is well justified for us to suggest a Mediterranean diet supplemented with either EVOO or nuts, as such diets are more likely to cause reversion of the condition.23
Another analysis of the data revealed that individuals in either of the MDP groups (EVOO or nuts) had lower glycemic loads and lower glycemic indexes than the low-fat control group.24 Thus it’s no surprise that even just 1 year of adding EVOO or nuts to a MDP diet is associated with lower blood pressure, reduced total cholesterol, and lower fasting glucose.25 As Lasa et al reported, “Mediterranean diets supplemented with virgin olive oil or nuts reduced total body weight and improved glucose metabolism to the same extent as the usually recommended low-fat diet.”26
Increasing Benefit
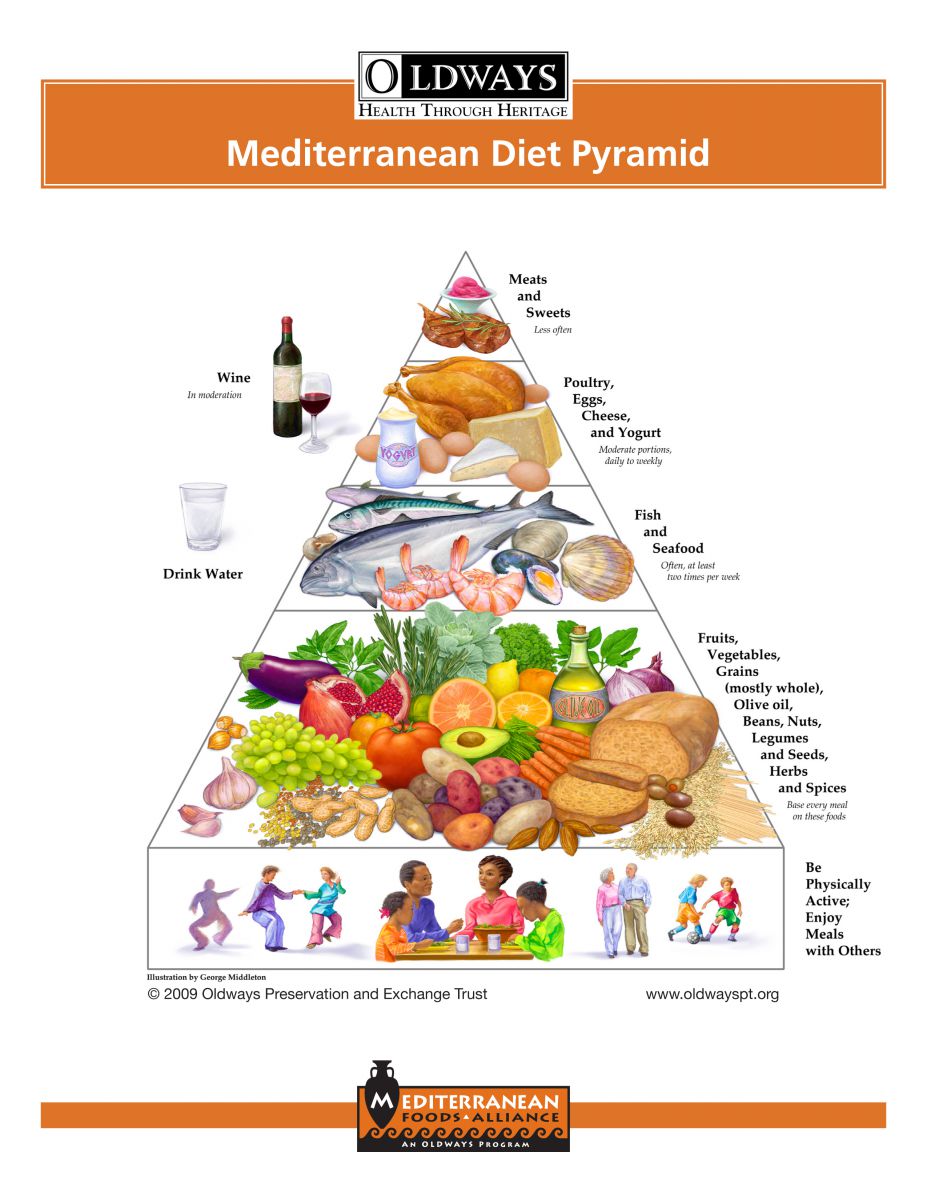
While following a basic MDP is useful, PREDIMED gives us solid evidence that we can enhance the benefit with just a few alterations: (1) switching from common olive oil to EVOO; (2) increasing consumption of nuts, fatty fish, and whole grain cereals; (3) reducing sodium intake; and (4) maintaining moderate consumption of wine with meals.26,27 (See the Figure for details of the Mediterranean diet.) The suggestion to eat whole grain cereals is further supported by a July 2013 study that reported “reducing white bread, but not whole-grain bread consumption, within a Mediterranean-style food pattern setting is associated with lower gains in weight and abdominal fat.”28
Figure. Mediterranean Diet Pyramid
Further encouragement to drink wine with meals comes from a pair of 2012 studies that were published even before the main PREDIMED study, both suggesting that resveratrol and wine intake “were associated with beneficial changes in blood lipid profiles, fasting blood glucose (only resveratrol) and heart rate, suggesting that resveratrol intake via wine consumption might help to decrease CV risk factors”29 and that these “polyphenol-rich foods in the Mediterranean diet are associated with better cognitive function in elderly subjects at high cardiovascular risk.”30
Specific Foods and Nutrients
Ongoing reports from the PREDIMED data also provide guidance on specific nutrients and foods that were not hinted at in the original analysis.
Fiber
Fiber is important. A study published December 2014 found that higher baseline fiber and fruit consumption among study participants was associated with a lower risk of death. Comparing the upper quintile against the lower quintile of consumption for fiber and fruit yielded 37% and 41% lower HRs for mortality respectively [HR:0.63; 95% CI:0.46-0.86; P=.015 and HR:0.59; 95% CI:0.42-0.82; P=.004). Participants who ate more than 210 g fruit per day had 41% lower risk of all-cause mortality (HR:0.59; 95% CI:0.44-0.78).31
Iron
Iron metabolism turns out to be an important predictor of diabetes. During the PREDIMED trial, 153 participants developed type-2 diabetes. They were compared with participants without diabetes who served as controls: 2 individuals matched by age, sex, body mass index, and intervention group were selected to serve as controls for each person who developed diabetes. Individuals with elevated serum ferritin levels (>257 μg/L in males and >139 μg/L in females) had a significantly increased overall risk for type 2 diabetes (OR:3.62; 95% CI:1.32-19.95; P=.022).32
Another study published in November 2013 reported a significant direct association between the incidence of type-2 diabetes and consumption of heme iron (HR:1.30; 95% CI:1.02-1.66).33 The same study also reported a slight reduction in risk associated with coffee consumption (HR:0.93; 95% CI:0.89-0.98) and an increase with consumption of alcoholic beverages (HR:1.02; 95% CI:1.01-1.04).33 Heme iron is derived from hemoglobin and is found only in blood containing animal-derived foods, what we call “red meat.”
Magnesium
Mortality among study participants, again all people at high risk for CVD, shifted with magnesium levels. After excluding participants with either high or low calorie intakes, 7,216 participants were included in this subset. Compared with participants with low magnesium intake, individuals in the highest tertile of magnesium had a 34% reduction in mortality risk (HR:0.66; 95% CI:0.45-0.95; P<.01). Individuals in this upper tertile of magnesium intake ingested about 454 mg magnesium per day.34 Thus it makes sense that we suggest that patients at risk for CVD take about this much magnesium per day (including dietary intake) along with a MDP.
Polyphenols
There is evidence now to support a theory that polyphenols are responsible for at least some of the benefit of Mediterranean diets. A May 2014 reanalysis of the PREDIMED data “found a 37% relative reduction in all-cause mortality comparing the highest versus the lowest quintiles of total polyphenol intake (HR=0.63; 95% CI 0.41 to 0.97; P-trend=0.12).”35 Among the polyphenol subclasses, stilbenes and lignans were significantly associated with reduced all-cause mortality (HR:0.48; 95% CI:0.25-0.91; P-trend=.04 and HR:0.60; 95% CI:0.37-0.97; P for trend=.03, respectively), with no significant associations apparent in the rest (flavonoids or phenolic acids).35 Total polyphenols are associated with NO production and lowered blood pressure.7
According to a 2013 paper, in Spain the main dietary sources of polyphenols are coffee and fruit, “but the most important differentiating factor with respect to other countries is the consumption of polyphenols from olives and olive oil.”36 The mean total polyphenol intake among study participants was 820±323 mg per day.36 Even 1 year into the trial, participants assigned to 1 of the Mediterranean diet groups, either with EVOO or nut supplementation, had higher total plasma antioxidant capacity than those in the low-fat control group.37
Vitamin K
Vitamin K levels in the diet may also have a significant impact on health. Researchers reported in May 2014 that “Dietary intake of vitamin K is inversely associated with mortality risk.”38 Baseline dietary phylloquinone (vitamin K1) intake was associated with a significant 46% reduced risk of cancer and all-cause mortality after controlling for potential confounders (HR:0.54; 95% CI:0.30-0.96; and HR:0.64; 95% CI:0.45-0.90, respectively). Study participants who increased their intake of phylloquinone or menaquinone (vitamin K2) during follow-up had a lower risk of cancer (HR:0.64; 95% CI:0.43-0.95; and HR:0.41; 95% CI:0.26-0.64, respectively) and all-cause mortality (HR:0.57; 95% CI:0.44-0.73; and HR:0.55; 95% CI:0.42-0.73, respectively) than individuals who decreased or did not change their intake. In addition, individuals who increased their intake of dietary phylloquinone had a lower cardiovascular mortality risk (HR:0.52; 95% CI:0.31-0.86). However, no significant association between changes in menaquinone intake and cardiovascular mortality was observed (HR:0.76; 95% CI:0.44-1.29).38 Additionally, the PREDIMED data revealed in a January 2013 report that “phylloquinone intake is associated with an improvement of cytokines and other markers related to insulin resistance and diabetes, thus extending the potential protection by dietary phylloquinone on chronic inflammatory diseases.”39
Brain Benefits
Following a MDP appears to affect more than general health. Adherence is associated with greater psychological health and cognitive function.
A May 2014 paper reported that “prevalence of symptoms of depression and anxiety is high in patients with bronchiectasis, and greater adherence to a Mediterranean diet is associated with a lower likelihood of having these symptoms, particularly for depression.”40 A December 2013 paper reported that PREDIMED participants who were either in the EVOO group or the nut group scored better on various measures of cognitive function than did the control group.41During the original PREDIMED study, 224 new cases of depression were diagnosed. The participants assigned to the nut group had a nonsignificant 22% reduced risk of being diagnosed with depression than those in the control group (HR:0.78; 95% CI:0.55-1.10). This difference reached significance when restricted to participants who had type-2 diabetes. In diabetics, supplementing the diet with nuts was associated with a 41% reduced risk of being diagnosed with depression during the course of the study (HR:0.59; 95% CI:0.36-0.98).42 PREDIMED participants in the EVOO group also demonstrated better cognitive function in comparison with a control diet.43
Gout
The 14-item questionnaire used to score Mediterranean diet compliance also proved useful in identifying patients with gout:
An inverse association was observed between increasing levels of adherence to the 14-item MeDiet score and decreasing hyperuricemia (p trend < .001). Baseline consumption of red meat, fish and seafood, and wine were associated with a higher prevalence of hyperuricemia. . . .Reversion of hyperuricemia was significantly higher (multivariable-adjusted odds ratio=1.73; 95% CI:1.04-2.89) in the highest category of baseline adherence to the MeDiet as compared with the lowest.44
Gazpacho
Perhaps the most entertaining study to come out of the PREDIMED data is one that focused on gazpacho consumption. Gazpacho, of course, is a cold soup particular to Spain. Using the diet and food consumption data from the PREDIMED Trial, researchers reported in October 2013 that “Gazpacho consumption is associated with lower blood pressure and reduced hypertension. . . [and] was inversely associated with systolic and diastolic [blood pressure] and prevalence of hypertension in a cross-sectional Mediterranean population at high cardiovascular risk.”45 The study authors theorize this association “is probably due to synergy among several bioactive compounds present in the vegetable ingredients used to make the recipe.”45
Conclusion
When the PREDIMED results were first published, we had reason to question the broad interpretation that adherence to a MDP had as significant an impact as the authors claimed. While it was clear that supplementation with EVOO or nuts was associated with significant benefit, it was a stretch to find clear evidence for the dietary pattern in general because the actual diet followed by participants in the 3 original arms differed only slightly. However, subsequent analyses of the data have brought certainty to the broader claims that adherence to the Mediterranean diet itself can provide significant benefits: lowering the risk of CVD and stroke and reducing incidence of MetS, overweight, and overall mortality. The PREDIMED data suggest that both EVOO and nut consumption play an essential role in the health benefits of the Mediterranean diet. The depth of evidence supporting the Mediterranean diet continues to grow.
We should, whenever possible, encourage our patients to adhere to a Mediterranean patterned diet unless there are contraindications for specific aspects of the diet.